Recently I’ve been reading a book (published in 2004) by Betty O’Keefe and Ian McDonald titled, Dr Fred and the Spanish Lady. The work examines the experience of Dr. Fred Underhill, who was the senior public health officer in Vancouver during the 1918 pandemic. While there had been a host of influenza pandemics through history, the 1918 pandemic killed perhaps 100 million people globally.
What struck me while reading the work was the manifold similarities between our experience of COVID-19 and that of almost exactly a century before. During our current pandemic some countries, such as Australia, New Zealand and Taiwan, acted quickly to enact travel restrictions. But that was the exception rather than the norm. Similarly, in 1918 troop ships brought influenza to Canada, even though during the crossings the ships would have to repeatedly stop for the burial of sea for returning soldiers (O-Keefe and MacDonald, 30-31). In 1918, travel restrictions were not implemented because everyone in Canada wanted to bring the troops home. While understandable, this was also tragic. During COVID-19 there were no effective limits on returning citizens in the United States, likely because there just was not enough public support for this measure. Of course, there were limits on non-citizens’ travel. But since the SARS-Cov2 virus does not discriminate based on citizenship, those countries that did not limit their citizen’s movement, and quarantine them on arrival, have paid a heavy price.
There are many other parallels. In 1918 Canadian cities (such as Ottawa) enacted curfews (p. 64), as many other North American cities have done during COVID. But since SARS-CoV-2 spreads quite as effectively at all hours, and this measure does not change behavior while shops and public places are open, this measure proved to be as ineffective in 1918 as it seems to have been now.
Equally important, there were debates about mask wearing, and some people refused to wear them in 1918 (p. 69, 120), much as was the case -in the United States in particular- during COVID-19. Still, in general people seem to have respected public health authorities more during the 1918 pandemic, and masks did not become as politicized to the same extent that they did in places such as the Dakotas in 2020.
We have recently seen a trend away from 14 day quarantines with COVID towards a ten day one. In 1918 there were bitter fights about quarantine, about everything from its length, to the fact that people saw that their neighbors were not observing it (71). There were also a host of fake remedies for the disorder, much like the early enthusiasm for hydroxychloroquine with COVID-19 (71). These remedies reflected the popular desperation for a cure. As someone who has spent much of the last 15 years studying conspiracy theories in public health, I believe that denial is central to most health-related conspiracies. People would much rather think that there is a cure that authorities are hiding, rather than believe that there is no well-documented treatment tyet for an illness, a much scarier proposition. Of course, the popular remedies in 1918 were more likely to involve ingredients such as onions. But how did putting sulpher in your shoes become a thing (p. 85)?
In the early stages of the pandemic in 1918 people were told that it was a short lived disease (p. 74), and that one could recover quickly (74). The terrible story of encephalitis lethargica was far in the future. Similarly, with COVID-19 people believed that if you survived that you would recover quickly. For this reason, the first sufferers of long-COVID often experienced skepticism not only from their doctors but also from their families and friends.
Perhaps the greatest similarities between the two pandemics were with the serious debates about municipal closures (p. 79). Should people be informed of the risks and left to make their own decisions based on their free will (82). In 1918 people begged public health authorities to keep churches open for events such as marriages (80). In Victoria, BC, their requests were refused. In the end many church services moved outdoors (p. 134). The debates about keeping schools open were particularly difficult in Vancouver, because Underhill (p. 81) -like many public health officials- worried what would happen to children if they did not have schools to go to. Businesses -and even newspapers- said that people were being unnecessarily frightened (p. 88). At the same time, nervous politicians heard from voters who were unhappy that there were not closures (92). With time, the calls to lift restrictions became increasingly strong (129), especially once the death rate began to diminish.
Perhaps because they worried that people might panic, some public health officials tried to minimize the danger by saying that even a good rain would help to clean the air (97). One doctor advocated against closures because “human psychology gives idle people time to believe they are sick when they are not (103). I don’t think that I would have wanted him as my doctor.
Some of the advice given sounds decidedly modern, such as the emphasis on proper ventilation and isolating the ill within the family (p. 83). There was a lot of discussion of the importance of fresh air, and keeping windows open. Boarding houses -and other places where people were densely housed- saw particular high attack rates (p. 92). In 1918 some public health authorities wanted to immediately take the sick out of housing and to the hospitals, in order to protect their families.
One of the key questions was to hold major events such as War Bond Rallies (p. 93). These often went forward, much like the Superbowl parties in West Florida, or the Australian Open. In 1918, the results were often devastating. Another issue was the extent to which different government authorities would cooperate. In 1918 there were intergovernmental disputes in the lower BC mainland in Canada (98), or just a lack of cooperation. Of course, in the spring of 2020 there were struggles between state and federal authorities about access to such items as personal protective equipment. In both pandemics, there was a desperate shortage of medical workers (124).
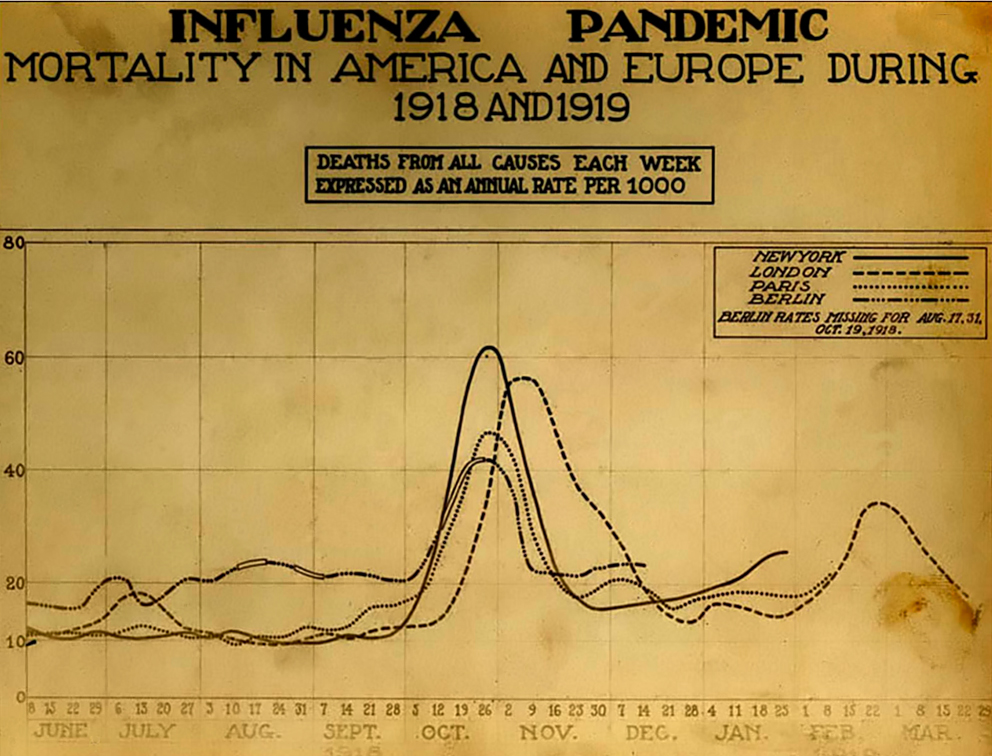
Interestingly, influenza seemed to become less dangerous with time, much as mortality rates have declined in North America with COVID-19 (p. 119). Still, the pandemic lasted a great deal of time, although it faded away in 1919. Sadly, pandemics can sometimes last a very long time, as one terrible multi-species pandemic in prehistory proves, as it lasted fifteen million years. It’s left its terrible traces in the genomes of widely different species. Hopefully, COVID-19 will fade away in a few years with vaccines.
In the end, people seemed to have managed the 1918 pandemic at least as well, and often better, than many authorities have dealt with the COVID-19 outbreak. In 1918 there were bitter debates about public health policy. But public health measures generally did not become as politicized then as they did in the US with COVID-19. Of course, in 1918 they did not have certain resources, such as apps to help with contact tracing. But in many countries -such as the United States- these apps have been almost unused for political reasons, which meant that effectively public health authorities had to rely on the same tools as a century ago. Of course, the key difference between then and now was that now we have effective vaccines. Hopefully, this will create a different end to the COVID-19 pandemic.
There might be one other similarity between the two pandemics. As the pandemic faded, people celebrated the end of the war and the return to normal life (134). Entertainers had been among the groups that had suffered the most during the pandemic, but people went right back to hear music and see plays as soon as the influenza outbreak passed (p. 140-142). But medical personnel -including doctors- had been psychologically scarred by what they had seen. I wonder if after COVID-19 the memory of the pandemic will fade among the public, while doctors, nurses and others will continue to be haunted by their experiences. As Alfred Crosby and others have argued, the 1918 pandemic was one that people were eager to forget. How will our pandemic be remembered? And what aspects of the pandemic will be forgotten? And when the next pandemic comes will we remember the lesson of 1918, that the areas and nations that did better were those that shut down early and hard (p. 154-155)?
References:
Crosby, Alfred W. (2003, originally 1976). America’s Forgotten Pandemic. West Nyack: Cambridge University Press.
O’Keefe, B., & Macdonald, I. (2004). Dr. Fred and the Spanish lady: Fighting the killer flu. Heritage House Publishing Co.
Full disclosure: Heritage House Press also published my book on the windigo.