The warning signs in Hong Kong
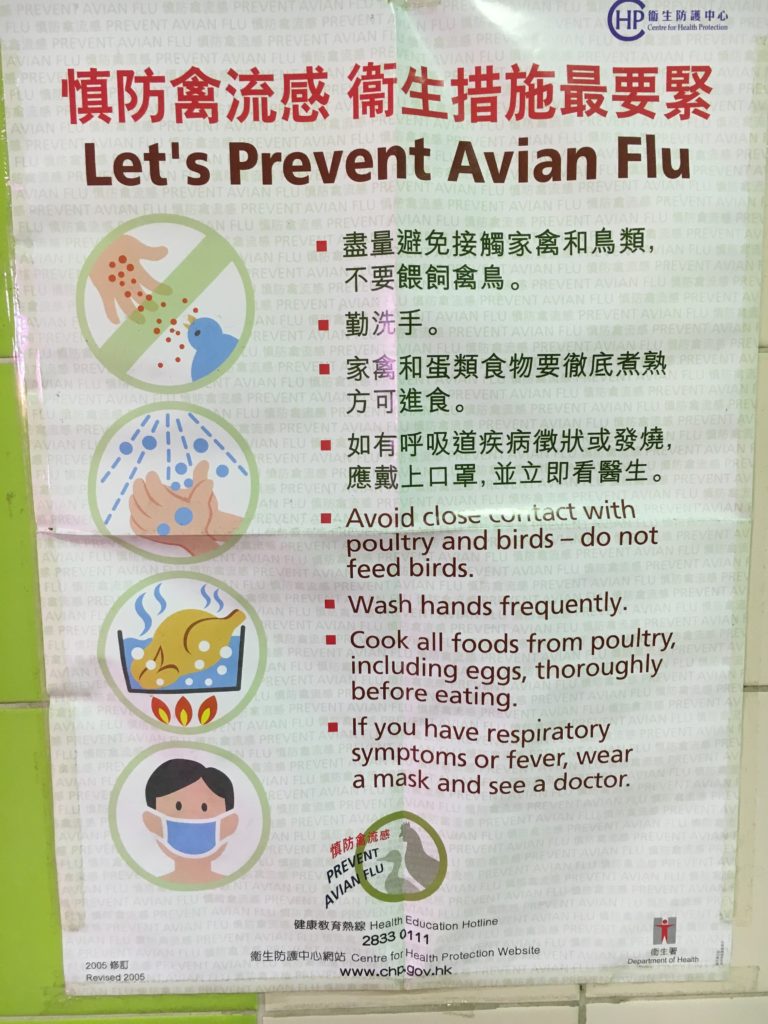
In 2017 I traveled to Hong Kong to do research for a paper about the pandemic risks posed by wet markets (marketplaces which sold and slaughtered live animals). I traveled to wet markets large and small, and took notes on their practices and clientele. I also interviewed public health experts and doctors about the territories system to control avian influenza in poultry.

While in Hong Kong, I also traveled to Macau and Shenzhen. When I crossed into mainland China, I was struck by the extent to which information was restricted. It’s one thing to know that China has a separate digital ecosystem. It’s another to no longer be able to use Google Maps, and to know that there’s no point in even trying to use a VPN to connect with websites at home. When I arrived in Shenzhen, I found this card in my hotel. You couldn’t access your files in Google Drive, check Twitter, watch a YouTube video, or see your kids’ posts on Instagram. The Great Firewall of China is both pervasive and efficient.
While I was in Hong Kong, I also had an opportunity to talk to someone whom I greatly respected. At one point in our discussion they asked me “Do people see what is happening here in Hong Kong? Are they following what is happening here?” I said that no, in my opinion most Americans did not. In the United States people were focused on the new presidency of Donald Trump. She/he seemed very disappointed by my answer, and asked the same question again with slightly different wording. I gave the same answer. In 2017, I don’t think most Americans -and perhaps most Europeans- were carefully following what was happening in Hong Kong. That would change over the next year and a half. …

 I am fortunate to be a Taiwan Fellow this fall. I plan to study Taiwan’s response to the COVID-19 outbreak at National Taiwan University starting this September, where I am being hosted by the global health program. I just received my visa to travel to Taiwan last week. Unfortunately, there is currently a growing outbreak in Taipei. I first heard of it last week, when I was talking with my conversational partner in Taiwan. At that time, she said that the outbreak was still relatively small, as it involved perhaps thirty individuals. But this morning I had an email and a text -the latter of which was sent to everyone who recently received a visa- to say that Taiwan is halting all travel to the island, except for residents. I am hopeful that Taiwan will soon have the situation back under control. But what happened?
I am fortunate to be a Taiwan Fellow this fall. I plan to study Taiwan’s response to the COVID-19 outbreak at National Taiwan University starting this September, where I am being hosted by the global health program. I just received my visa to travel to Taiwan last week. Unfortunately, there is currently a growing outbreak in Taipei. I first heard of it last week, when I was talking with my conversational partner in Taiwan. At that time, she said that the outbreak was still relatively small, as it involved perhaps thirty individuals. But this morning I had an email and a text -the latter of which was sent to everyone who recently received a visa- to say that Taiwan is halting all travel to the island, except for residents. I am hopeful that Taiwan will soon have the situation back under control. But what happened?