A new COVID-19 variant
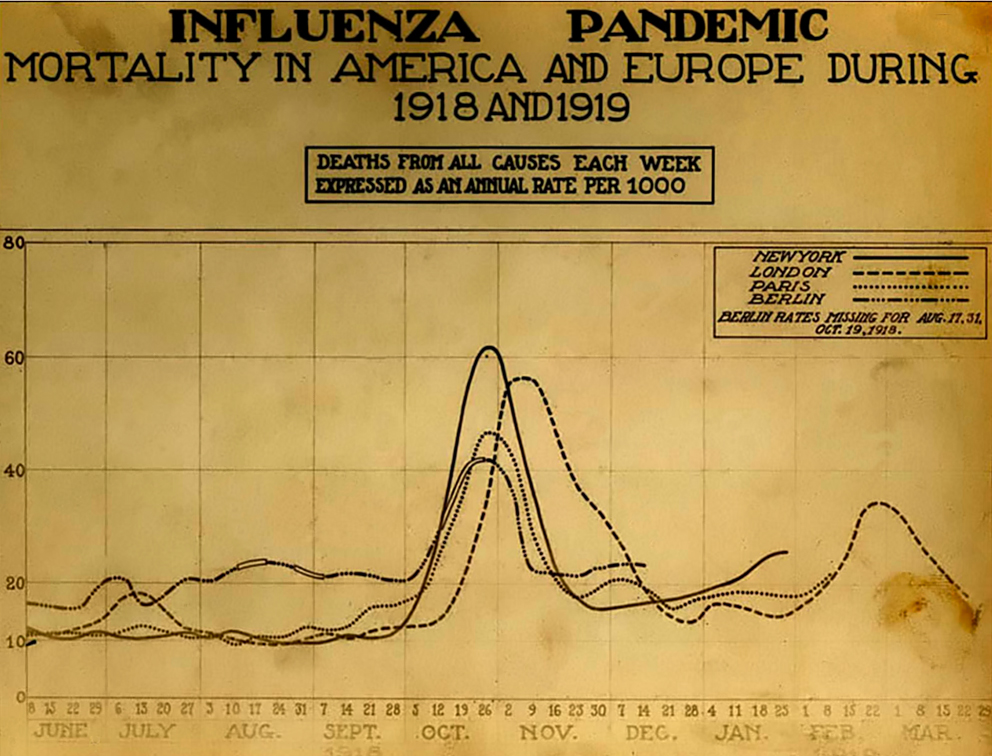
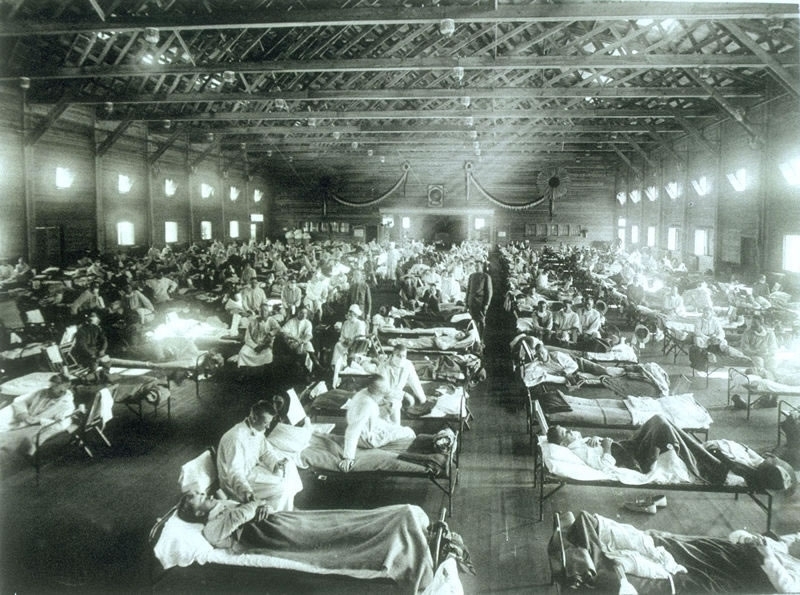
Early in the pandemic I thought it likely that COVID-19 would have multiple waves, perhaps three like the 1918 influenza pandemic. So I never thought that the pandemic would end quickly. But over the last six or seven months I keep finding myself thinking that this time, finally, it must be ending. In June I had both of my COVID-19 vaccinations, cases in the US were plummeting, and I thought that by this winter it would have finally ended. Then Delta arrived, and filled the emergency rooms of the US south. This fall I was able to travel to Lisbon, where I am carrying out historical research on the 1918 influenza pandemic. When I arrived this October Portugal was the most vaccinated country in Europe, and was the subject of a front page article in the New York Times. And yet since I’ve arrived I’ve seen the case right rise dramatically. Not long ago I was looking at the New York Times country data page, and saw that cases in Portugal had increased 116% in two weeks. The country’s case rate may pass that of the US before long. Keep in mind that not only does Portugal have a high vaccination rate, but also people are very good about wearing masks here. It’s common to even see people wearing them in the street, at least if the street is crowded.
While Portugal is facing serious challenges, the situation is far better here than it is in other places, such as Austria. The COVID-19 incidence there is growing at a stunning rate. The government is implementing firm measures, but is facing mass protests. Other countries, such as the Netherlands, are in the same situation, as we have seen from the protests in Rotterdam. Still, the situation is much worse in Eastern Europe, where in some countries such as Bulgaria only a quarter of adults are vaccinated.
It’s in this context that we are receiving news about a new -as yet unnamed- variant in South Africa. There is a lot that we don’t know about this variant yet. The German news channel recently interviewed one expert who suggested that it might be 500 percent more infectious than Delta, although he stressed that we just don’t know yet. Even such qualified statements are dangerous. We will have more data soon. Still, there is a lot of speculation that this variant might partially evade vaccines, because there are so many mutations, including a number involving the virus’s spike protein.
Nations are rushing to block flights from South Africa. Britain was very slow to respond to the Delta variant, and allowed travel to continue for weeks after it was clear that Delta might lead to a new wave. But after the news of this new variant emerged Britain blocked air travel from Southern Africa. Many other nations are also imposing travel restrictions. Of course, this variant has already been found in Israel. And in Hong Kong -where it was brought by a traveler from South Africa- it managed to spread to one other person in a quarantine hotel. Blocking travel from South Africa will help to buy some time, which might be put to use gathering data on the virus. It might also give people the time to be fully vaccinated and get their boosters, if they are in countries in which vaccines are readily available. But in the end, it won’t be enough. Without a complete border and air travel shut down, a highly infectious virus will certainly spread globally.
Given that Delta is already so severe in Europe, the timing for the emergence of this variant could not be worse for this region as it heads into winter. People are exhausted from the pandemic. But it’s not over. Please, if you are not vaccinated, hurry to be vaccinated now, so that your body has time to build immunity. While all medical treatments have risks, the risks of COVID-19 are much greater, billions of people have had the vaccines, and a new variant is coming. And if you are eligible for a booster, now would also be a good moment for that too. Two months ago there was a significant debate around whether boosters were necessary. Given what’s happening now in places like Portugal, there’s no doubt that only focusing on the severity of cases, and not on transmission, is a poor public health approach.
Let’s hope that this proves to be a false alarm, and that the new variant doesn’t greatly increase severity, transmission, or vaccine evasion. We all deserve some luck.